|
The Coordination and Support Action (CSA) HEcoPerMed responds to the demand for economic models that evaluate treatments made possible through innovations in Personalised Medicine (PM). With our 2nd newsletter, we inform you about our events as well as the latest developments in our academic research, which aims to contribute to the timely uptake of cost-effective PM innovations.
HEcoPerMed Hybrid-Workshop and outlook to the final conference on 28 April 2022
The HEcoPerMed workshop 'Personalised Medicine Specific Health Economic and Payment Modelling' was conducted as a hybrid event in Budapest in October 2021. During this by-invitation-only event the results and achievements of the consortium were presented.
Furthermore, the first draft of a position paper entitled 'Personalised Medicine: Using Health Technology Assessment to Choose Wisely' was presented and discussed with around 70 international experts and stakeholders, who were present on-site or online.
The position paper will be launched at a final conference that will take place in Brussels on 28 April 2022, on-site by invitation only, and with online streaming. In addition, we will present our overall achievements and results at the conference. Through moderated discussions, the outcomes of the project will be placed into the policy context. The position paper will be made available also on the HEcoPerMed website.
For further information, find the agenda and report of the Budapest workshop on the HEcoPerMed website.
More...
Four Future Scenarios for Personalised Medicine
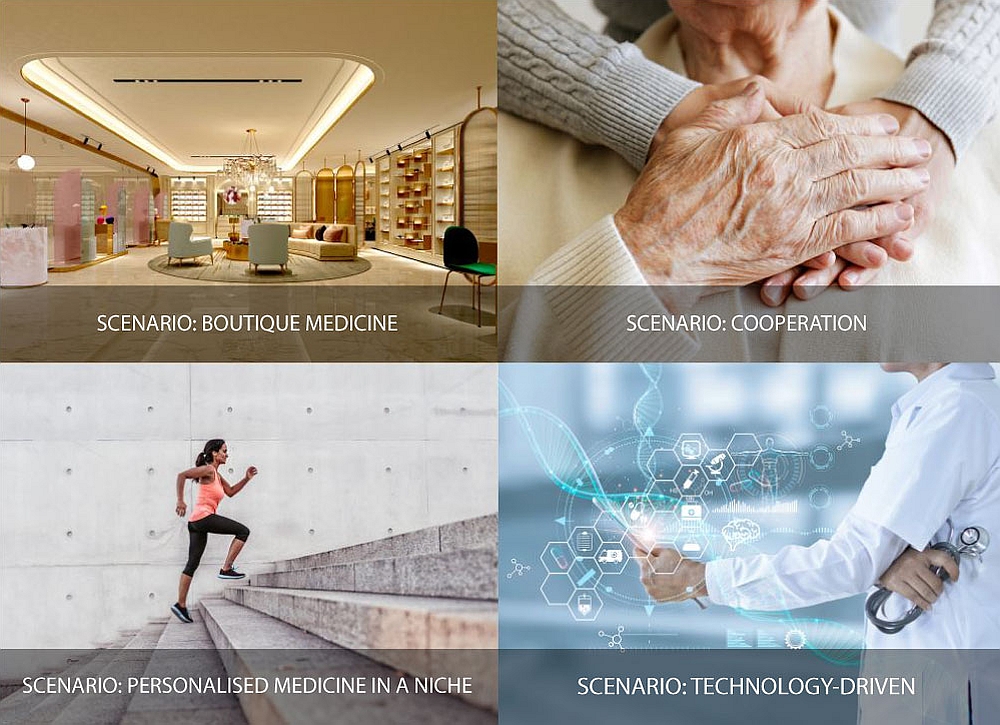
The aim of the HEcoPerMed scenarios is to tell parallel stories of what different futures of Personalised Medicine might look like from a wider societal perspective. The scenarios are by no means predictions. Rather, the scenarios developed represent plausible alternatives in which different aspects dominate. Scenarios create links between future assessments (i.e., trends, drivers) of a variety of stakeholders and participants in the scenario process and can thus create pictures of the future with greater density and diversity, going far beyond a stringing together of individual trends. Linking trends and drivers in scenarios makes framework conditions and critical issues visible where development could go in different directions. This perspective is especially important for policy makers. The HEcoPerMed scenarios differ in the roles of actors and institutions, beneficiaries, funding mechanisms and, in particular, the integration of personalised medicine into the healthcare system.
Scenario 1 'Privatisation – Boutique Medicine vs. Automated Medicine':
Healthcare is largely privatised. The public sector has retreated from supporting a tax-based health system due to ever rising costs. Personalised Medicine is something for wealthy people who do 'health shopping' on an international scale. Most of the investments for Personalised Medicine comes from the private sector.
Scenario 2 'Technology-driven – Personalised Medicine by Subscription':
Public and private funds are available for technological progress including Personalised Medicine. Sharing one’s own data is the entry point to the healthcare system. Technology-driven medicine that uses e.g., the Internet of Things with sensors everywhere allows more flexible healthcare. Rapid decline in genome sequencing costs has made it affordable for everyone.
Scenario 3 'Cooperation – Personalised and Holistic Medicine':
Personalised Medicine advances through open and intense cooperation between all actors within the health sector: science, policy, insurance, pharma industry, SMEs, patient organisations. There is a worldwide exchange of health data. The population is quite healthy due to the excellent healthcare system. People are working longer and extending their working lives to finance healthcare.
Scenario 4 'Scepticism – Personalised Medicine in a Niche':
The society is increasingly questioning evidence-based healthcare and has little trust in data-driven health-care systems due to expected data breaches. The health insurance system is solidarity-based but does not provide much funding for advanced medical research, treatment, or Personalised Medicine.
More...
23 Recommendations in Modelling Precision Medicine: Learning from Case Studies in Tumour Agnostic Treatments, DPYD Genotyping and Maturity Onset Diabetes of the Young
23 recommendations for the health economic modelling of PM were published by the HEcoPerMed consortium in 2021 and presented during a workshop at the ISPOR Europe 2021 virtual conference. You can access the publication describing the recommendations here.
Eight recommendations were aimed toward the accurate modelling of testing pathways, given the importance of patient stratification in PM. Five recommendations dealt with the estimation of treatment effectiveness, which may be complicated by the small patient groups in PM. Remaining recommendations discuss structural uncertainty and additional value elements, among other topics.
Three case studies were used to demonstrate solutions to the challenges of health economic modelling of Personalised Medicine (PM):
- Tumour-agnostic treatments for NTRK fusion-positive (NTRK+) cancer
- DPYD genotyping prior to fluorpyrimidine-based chemotherapy for personalised dosing (ToxNav)
- Screening for maturity onset diabetes of the young (MODY)
The health economic model for NTRK+ cancers illustrates how to estimate comparative effectiveness for single-arm basket studies (including how to account for the prognostic value of a genetic marker), and how to account for the risk of death while waiting for (genetic) test results. The model also shows the effect of incorporating the testing that is needed to identify patients eligible for a new treatment, as opposed to only modelling the treatment of eligible patients. The MODY case demonstrates the importance of patient stratification, test positioning and predictive accuracy, and the impact that detecting heritable mutations may have on relatives. The ToxNav model illustrates how to incorporate physician compliance and clinical decisions in real-world settings.
During the ISPOR workshop, the participants discussed the appropriateness of the solutions we used in our case studies, guided by the 23 recommendations for modelling PM. Participants also discussed the discrepancy between data needs for EMA approval versus data needs for health economic modelling to support reimbursement decisions.
More...
New publication in Value in Health: 'The Net Benefit of Personalised Medicine: A Systematic Literature Review and Regression Analysis'
Previous reviews on the cost-effectiveness of Personalised Medicine (PM) have found that most PM interventions increase costs and health benefits. They have also found large heterogeneity in outcomes. We expand on previous research by focusing on incremental net monetary benefit (ΔNMB) as opposed to incremental cost-effectiveness ratios, which allows for easy ranking of the interventions and for assessing the magnitude of their benefit. We explore the heterogeneity in outcomes using regression analysis.
PM interventions were found to have modest health benefits compared with non-PM. Nevertheless, its costs tend to result in 0 to negative ΔNMB on average. Gene therapies were found to have larger health benefits than other PM interventions. Nevertheless, they were also associated with higher costs and significantly lower ΔNMB, though this finding was sensitive to (small) data changes and hence uncertain. PM interventions for neoplasms had lower Δcosts and larger ΔNMB than PM interventions for other conditions, yet average ΔNMB in the 'neoplasm' group was still negative. Pricing policies may be needed to reduce the costs of gene therapies and other interventions with negative ΔNMB.
Beyond the difference between gene therapies and other PM interventions, no statistically significant factors could be identified to explain the large heterogeneity in cost-effectiveness outcomes. It appears that the term 'Personalised Medicine' may be too general given that it conceals sizable differences in the net benefit of different PM interventions. A more precise division into subcategories of PM may be needed to uncover the most promising areas for further investment.
More...
|